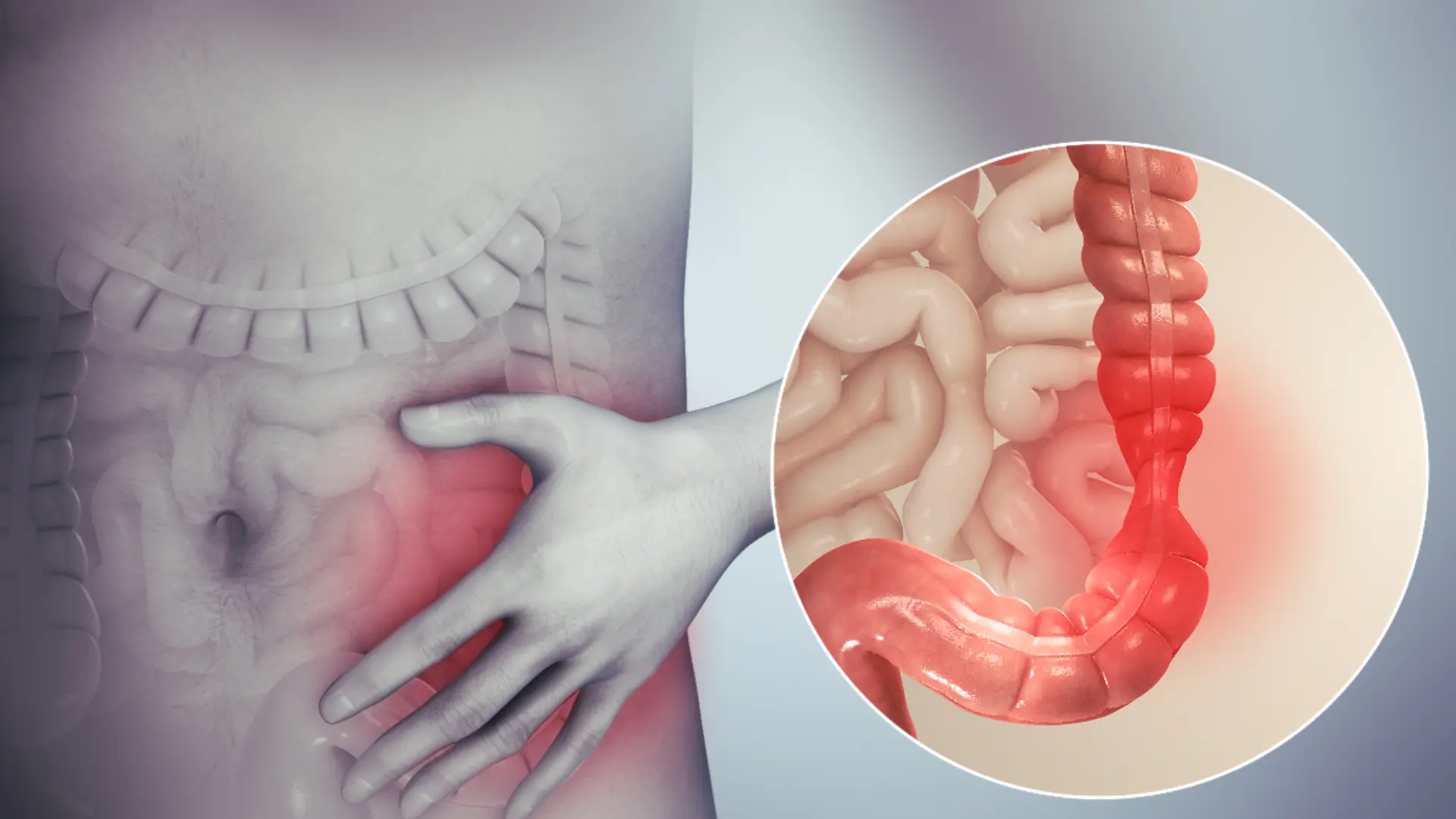
Understanding how FODMAPs affect digestive health is crucial, especially for individuals managing Inflammatory Bowel Disease (IBD). The Low FODMAP diet, which focuses on reducing specific short-chain carbohydrates that can cause digestive discomfort, has shown potential benefits for IBD patients.
By delving into the science behind FODMAPs and how they can trigger issues such as bloating, gas, and pain, this piece will provide valuable insights. Furthermore, it emphasizes the importance of consulting healthcare providers before making dietary adjustments and offers practical advice for incorporating low-FODMAP foods into daily meals.
Get ready to explore effective strategies and solutions for maintaining this diet long-term to improve your digestive health.
What Are FODMAPs?
FODMAPs, an acronym for Fermentable Oligo-, Di-, Mono-saccharides, and Polyols, are specific types of short-chain carbohydrates that can be difficult for some people to digest. Found in a variety of foods, including certain fruits, vegetables, grains, and dairy products, FODMAPs can ferment in the gut during digestion.
This fermentation process can lead to the production of gas and draw water into the intestines, causing symptoms such as bloating, pain, and diarrhea. For individuals with conditions like Inflammatory Bowel Disease (IBD), these symptoms can be particularly troublesome.
Therefore, understanding and managing the intake of high-FODMAP foods is essential for reducing digestive discomfort. It’s important to note that not everyone is sensitive to FODMAPs, and the degree of sensitivity can vary greatly among individuals. Consulting with a healthcare provider is recommended before making any dietary changes.
The Low FODMAP Diet
The Low FODMAP diet is a research-backed approach aimed at alleviating common digestive issues associated with high-FODMAP foods. Understanding the core principles and benefits of this diet can greatly assist in managing symptoms effectively.
In this section, we’ll explore the fundamentals and advantages of adopting a Low FODMAP diet, with special attention to its application for individuals with Inflammatory Bowel Disease (IBD).
Principles of the Low FODMAP Diet
The Low FODMAP diet is designed to minimize the intake of specific short-chain carbohydrates that can cause digestive issues. This diet is typically divided into three phases: elimination, reintroduction, and personalization.
In the elimination phase, all high-FODMAP foods are removed from the diet for a period of four to six weeks. This helps to reduce symptoms and provides a clear baseline for assessing food sensitivities. The reintroduction phase involves gradually reintroducing high-FODMAP foods one at a time to identify which specific types trigger symptoms.
Finally, the personalization phase tailors the diet to include only the FODMAPs that are well-tolerated, ensuring a balanced and varied intake of nutrients. For individuals with Inflammatory Bowel Disease (IBD), following these principles under the guidance of a healthcare provider can help manage symptoms and improve digestive health. This structured approach is supported by various inflammatory bowel disease trials and research studies.
Benefits for Digestive Health
The Low FODMAP diet has been shown to offer significant benefits for digestive health, particularly for individuals with conditions like Inflammatory Bowel Disease (IBD). By reducing the intake of high-FODMAP foods, many people experience a substantial decrease in symptoms such as bloating, gas, and abdominal pain.
Research has indicated that this dietary approach can improve overall gut health by promoting a healthier balance of gut bacteria. Additionally, various inflammatory bowel disease research studies have found that the Low FODMAP diet can help manage the frequency and severity of IBD flare-ups. Patients often report an enhanced quality of life and greater control over their symptoms.
However, it is crucial to follow this diet under the guidance of a healthcare provider to ensure nutritional adequacy and to tailor the diet to individual needs. The growing body of evidence from an inflammatory bowel disease trial underscores the potential long-term benefits of this dietary strategy.
Considerations for IBD Patients
For patients with Inflammatory Bowel Disease (IBD), adopting a Low FODMAP diet requires careful consideration and guidance from healthcare providers. While the diet can alleviate symptoms such as bloating, gas, and abdominal pain, it is essential to ensure that it does not compromise overall nutritional intake.
IBD patients often have unique dietary needs and may already be at risk for nutrient deficiencies. Therefore, it is crucial to work with a dietitian to create a balanced meal plan that meets individual nutritional requirements. Furthermore, the restrictive nature of the diet can be challenging to maintain over the long term. Ongoing support and monitoring are vital to make necessary adjustments and ensure sustainability.
Participation in Janssen IBD clinical trials and research studies can provide additional insights and personalized recommendations. Consulting healthcare providers before making dietary changes can help mitigate risks and optimize the benefits of the Low FODMAP diet for managing IBD symptoms.
Implementing a Low FODMAP Diet
Transitioning to a Low FODMAP diet may seem daunting, but it can be manageable and beneficial with the right approach. This section will provide practical tips, strategies to overcome common challenges, and long-term maintenance methods to help you seamlessly incorporate this diet into your daily routine. Whether you’re just starting or looking for ways to sustain your dietary changes, these insights will guide you toward better digestive health.
Practical Tips for Daily Meals
Incorporating low-FODMAP foods into daily meals can be straightforward with a bit of planning and creativity. Start by familiarizing yourself with high and low FODMAP foods. Keep a list handy to make grocery shopping easier. Meal prepping can also be beneficial; prepare low-FODMAP meals in advance to ensure you always have suitable options on hand.
For breakfast, consider low-FODMAP choices like oatmeal with lactose-free milk and a serving of berries. Lunch could be a quinoa salad with grilled chicken and a selection of low-FODMAP vegetables. For dinner, try roasted salmon with a side of steamed carrots and green beans.
Snacks such as rice cakes with peanut butter or lactose-free yogurt can help keep hunger at bay. It’s also essential to read food labels carefully to avoid hidden high FODMAP ingredients. Consulting with a dietitian can provide personalized meal plans and additional tips for maintaining the diet effectively.
Overcoming Dietary Challenges
Maintaining a Low FODMAP diet can present several challenges, but with the right strategies, these obstacles can be effectively managed. One common challenge is the restrictive nature of the diet, which can make it difficult to find suitable foods when dining out or traveling.
Planning by researching restaurant menus and carrying low-FODMAP snacks can help mitigate this issue. Another challenge is ensuring a balanced and nutritionally adequate diet. Working closely with a dietitian can help you meet your nutritional needs while adhering to the Low FODMAP guidelines.
Additionally, meal planning and preparation are crucial for success. Set aside time each week to plan your meals and batch cook to save time. Support from online communities and forums can also provide encouragement and practical advice. Lastly, be patient with the process. Gradually, you’ll become more adept at identifying and preparing low-FODMAP foods, making the dietary transition smoother over time.
Long-Term Maintenance Strategies
Maintaining a Low FODMAP diet over the long term requires strategic planning and consistency. One effective strategy is to keep a detailed food diary. Documenting what you eat and any symptoms you experience can help you identify and avoid specific high-FODMAP foods that trigger discomfort.
Regular consultations with a dietitian are also beneficial. They can help you adjust your meal plans to ensure nutritional balance and variety, preventing dietary monotony. Another key strategy involves gradually reintroducing high-FODMAP foods during the personalization phase to determine your tolerance levels. This allows for a more flexible diet while avoiding symptom triggers.
Staying informed about new research and updates can also be helpful, as ongoing inflammatory bowel disease trials and research studies continue to refine dietary guidelines. Lastly, leveraging support systems, whether through online communities or local support groups, can provide ongoing encouragement and practical advice for sticking to the Low FODMAP diet long-term.
Importance of Professional Guidance
Professional guidance is crucial when adopting a Low FODMAP diet, especially for individuals with Inflammatory Bowel Disease (IBD). A healthcare provider, such as a dietitian or gastroenterologist, can offer personalized advice tailored to your specific health needs. This professional support ensures that you maintain a balanced diet while avoiding high-FODMAP foods that trigger symptoms.
Additionally, healthcare providers can monitor your progress and make necessary adjustments to your meal plan, helping to prevent nutrient deficiencies and other potential issues. They can also interpret results from an inflammatory bowel disease research study and trials to provide evidence-based recommendations.
Consulting with a professional can help you navigate the complexities of the diet more effectively and sustain it long-term. Moreover, they can offer moral support and motivation, making it easier to adhere to the dietary guidelines. Overall, professional guidance is indispensable for optimizing the benefits of the Low FODMAP diet while safeguarding your health.
Final Thoughts
Understanding and managing FODMAP intake can significantly impact digestive health, particularly for individuals dealing with Inflammatory Bowel Disease (IBD). The Low FODMAP diet offers a structured, evidence-based approach to alleviating common gastrointestinal symptoms, improving quality of life, and promoting overall gut health.
However, it’s crucial to approach this diet with careful planning and professional guidance to ensure nutritional adequacy and long-term sustainability. By following the principles of elimination, reintroduction, and personalization phases, and incorporating practical strategies for daily implementation, individuals can successfully manage their symptoms.
Remember, the journey to better digestive health is a marathon, not a sprint. Patience, persistence, and support from healthcare professionals are key to making the Low FODMAP diet work for you. Stay informed, stay motivated, and take proactive steps towards a healthier, more comfortable life.
